
Frameworks for Respiratory Ethics
by Ian Goddard
Prior to Covid-19, who could have believed one day we would all be walking around wearing face masks? Masking for disease control in public had not been seen in most nations since the 1918 influenza pandemic. Then overnight there we were, all masking. My intuition was that being mandated to act so as to reduce the risk that I might spread a contagious novel virus that could kill millions before a vaccine was available was compatible with natural ethics, which is to say, it was compatible with what one ought to do under the extraordinary circumstances even in the absence of a mandate. However, how do I know that intuition about natural ethics was reasonable? Contemplating that question during the pandemic led me to the following ethical frameworks for respiratory hygiene.
Common air as common property
My immediate moral intuitions informed me that a body of terrestrial atmosphere, or air, serving as a common reservoir of life-sustaining oxygen is a common property of all its breathers. In other words, each breather has an equal co-ownership stake in that air. Why? Because each requires air to survive and it is naturally free worldwide. Therefore, if you have a right to life, you have a right to breathe that free air. Every breather, therefore, has an equal co-ownership stake in, and thus an equal right to access, the air around them.
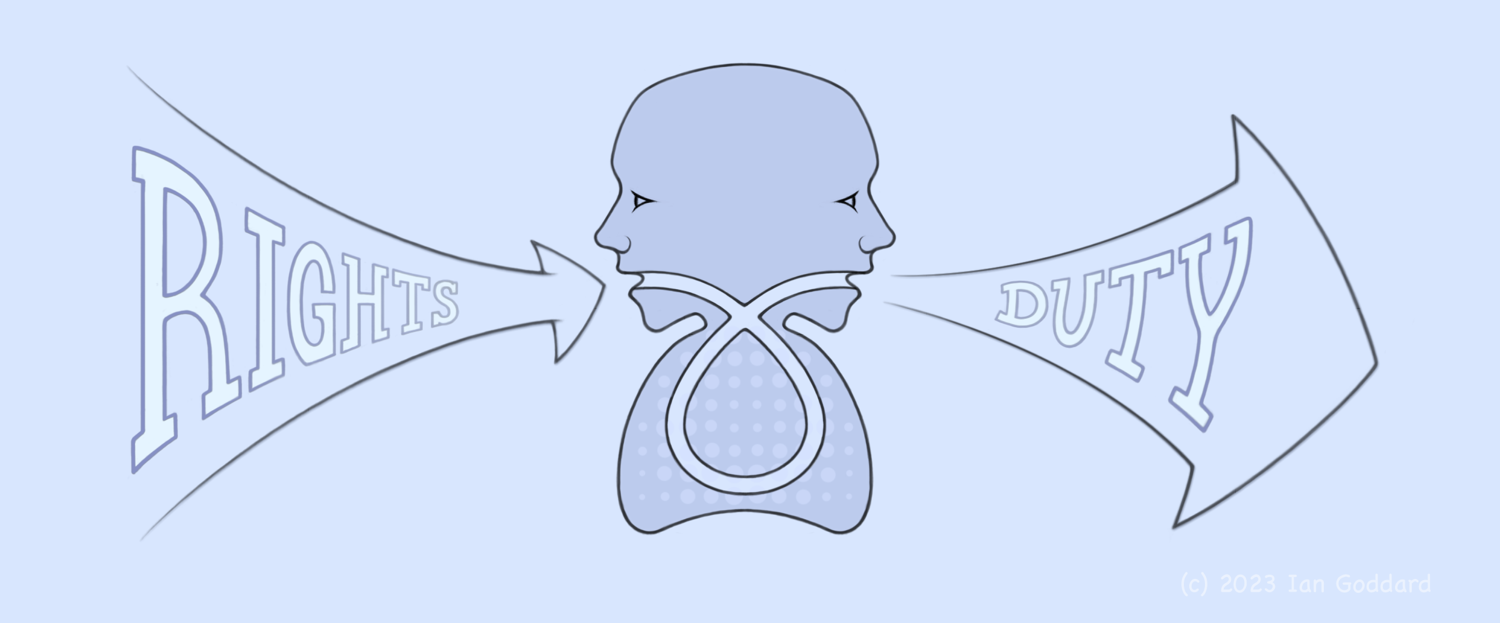
Following that reasoning, if a body of air is collectively owned by all its breathers, no single breather has a unilateral right to pollute it without the consent of the others. The air you exhale is likely to be inhaled by others given that they must inhale or die. So, for example, it is unethical to exhale cigarette smoke into the air that others breathe if they do not consent to inhaling it. Likewise, it is unethical to knowingly exhale harmful infectious germs into the air that others breathe if they do not consent to inhaling them. This is a logical framework of shared air that outputs moral rights and duties of breathers, as depicted in Figure 1.
There is, however, a more fundamental substrate for respiratory ethics than the common property of air. Polluting the air that others breathe is an ethical issue primarily because it is harmful. Even if we concluded that shared air can be privately owned, that would not entitle an owner of a body of shared air to physically harm others by polluting it any more than a landlord is entitled to physically harm their tenants, which of course they are not so entitled. Therefore, common ownership of air is a sufficient but not necessary condition for respiratory ethics. A more necessary fundamental substrate is harm and the ethical duty to not cause physical harm to the bodies of other people.
Non-harm undergirds respiratory ethics
From the Golden Rule to the Vedic principle of ahimsa to the Hippocratic Oath to the Lockean harm principle, the ethical precept that we should not cause harm to others, especially physical harm, endures from antiquity to this day. It seems, therefore, safe to say that knowingly causing physical harm to others with no justifiable reason is universally recognized as morally wrong, as something you ought not do. It is even recognized that accidentally causing physical harm to others incurs a moral obligation to compensate those injured thereby. One of the ways you can cause physical harm to the bodies of other people is by being a vector of an infectious disease and thereby spreading your infection to them.
Thanks to the discovery that contagious illnesses are spread by germs, we were able to determine measures to mitigate those illnesses. Such measures included water treatment, refuse management, food inspection and personal measures for respiratory hygiene such as not spitting in public places, washing hands and covering coughs and sneezes. After the discovery of germs, respiratory hygiene evolved from measures for personal health to include measures to prevent spreading harmful germs to others. And not just to prevent the harm an infectee might directly spread to others, but also harms that those whom they infected could in turn spread to others and so forth unto untold subsequent transmissions and magnitudes of aggregate harm.
Given the non-harm principle, this argument follows for every ‘you’ out there,
Premise: In accord with the non-harm principle, you should take precautions to prevent yourself from causing bodily physical harm to others.
Conclusion: Given that being a vector of an infectious pathogen can cause others to suffer mild to catastrophic bodily physical harm, according to the Premise, you should take precautions to prevent yourself from becoming such a vector.
This conclusion comports with social norms wherein since the dawn of germ theory we have been admonished to cover coughs and sneezes and stay home when sick. This norm is especially meaningful because the aggregate harm an infectee can cause by failing to prevent spreading their infection has an unknowable upward limit. The still-accruing aggregate harm unleashed by the one person who was the index case of Covid-19 includes millions of deaths, immeasurable suffering and economic loss worldwide to date. Even if you infect only one other person with the flu, that could lead to enormous downstream harm including sick leaves, medical costs and deaths among untold numbers of infections stemming from yours. When you have a respiratory infection, you have the power to prevent potentially massive aggregate human suffering by following the argument specified above.
A meta-framework for risk-mitigation frameworks
An important feature of risk mitigation is that risk varies over time. For example, the risk of harm someone poses to others increases when they are infectious with a contagious pathogen. It also increases when the likelihood that you are asymptomatically infectious rises during an epidemic wave. As the risk of harm we pose to others increases, our ethical obligation to prevent ourselves from causing that harm increases proportionally and in turn obliges us to use more effective measures to prevent that elevated risk. In this way, a duty to prevent harm and the measures taken to do so scale with changing levels of risk. This proportionality is depicted in Figure 2.
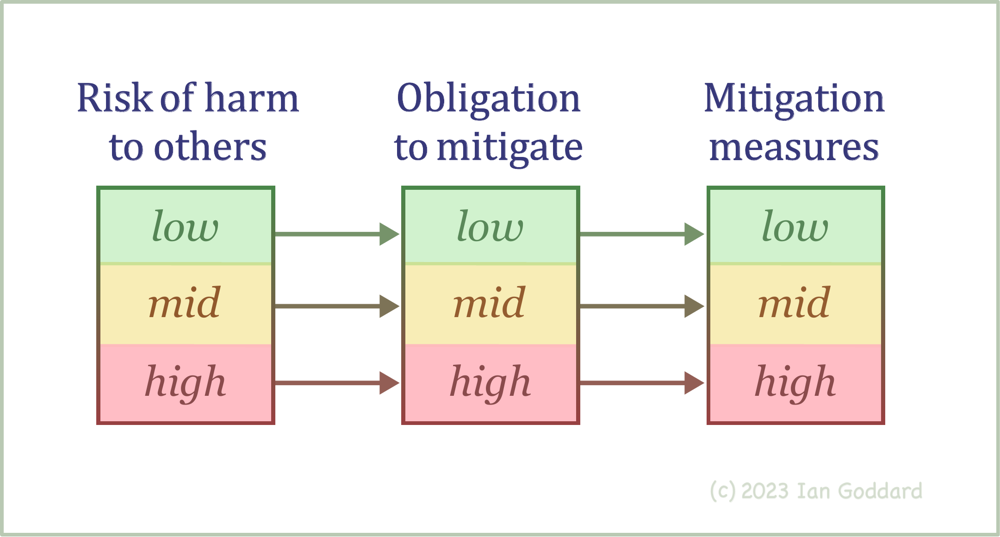
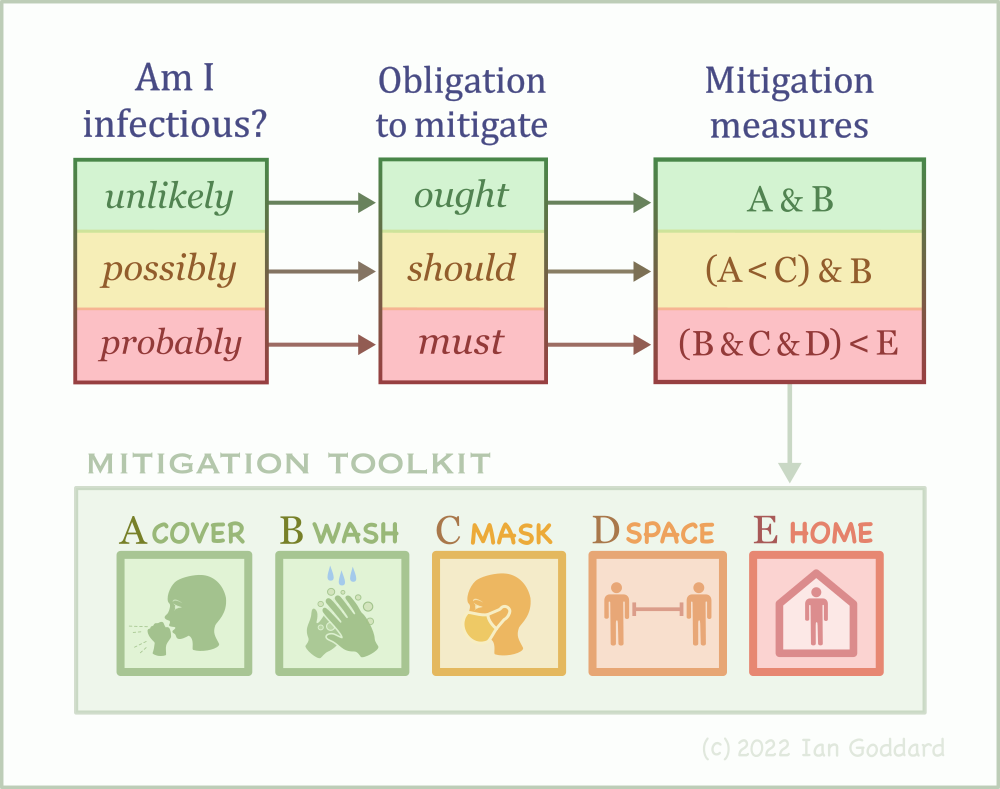
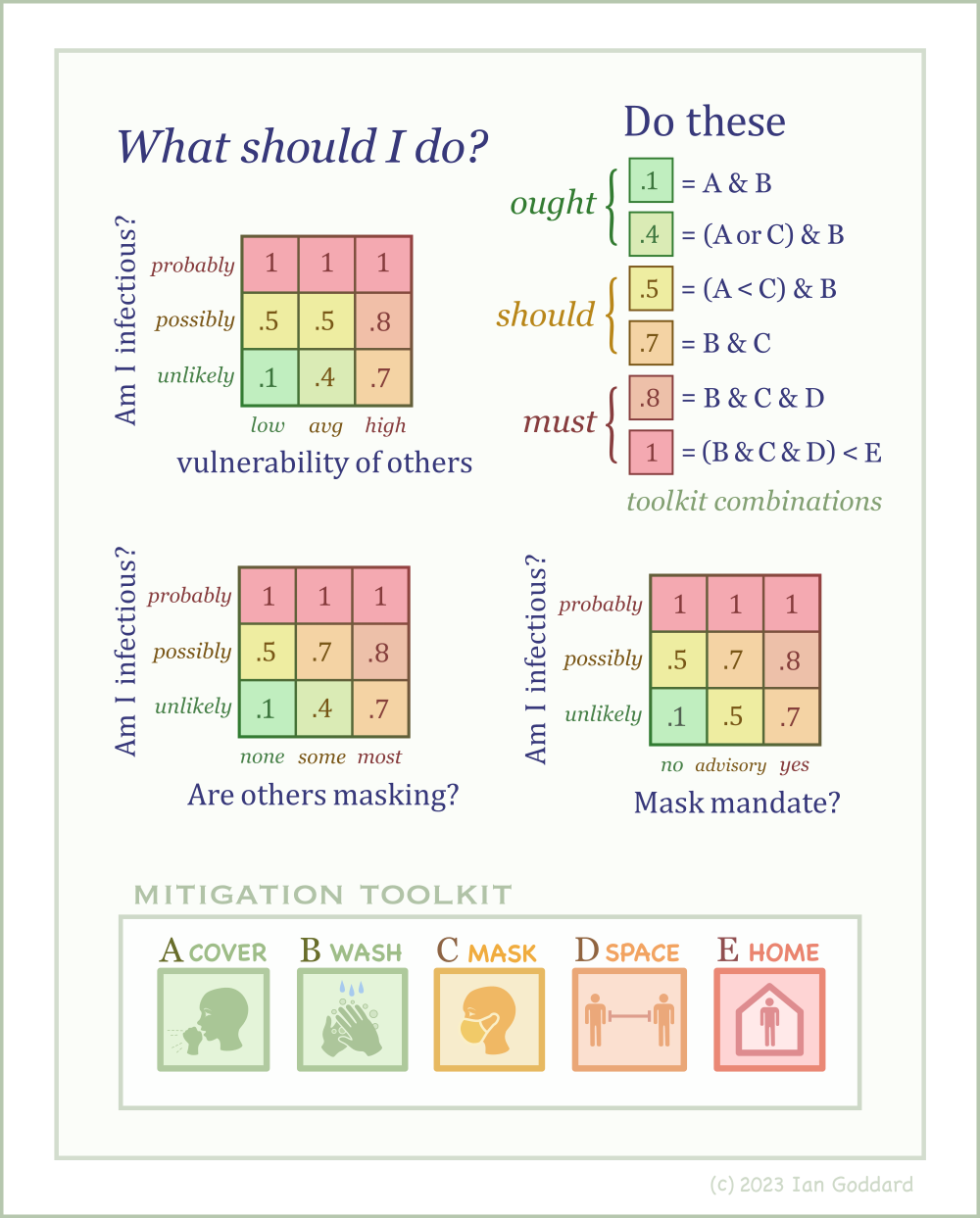
Figure 3 instantiates the framework in Figure 2 into the risk domain of respiratory hygiene and adds a mitigation toolkit for this domain. Other mitigation measures in this domain, such as ventilation and vaccination, could be included as well. This toolkit is not intended to be comprehensive but rather an example of how mitigative measures are scaled and layered in proportion to changing levels of risk.
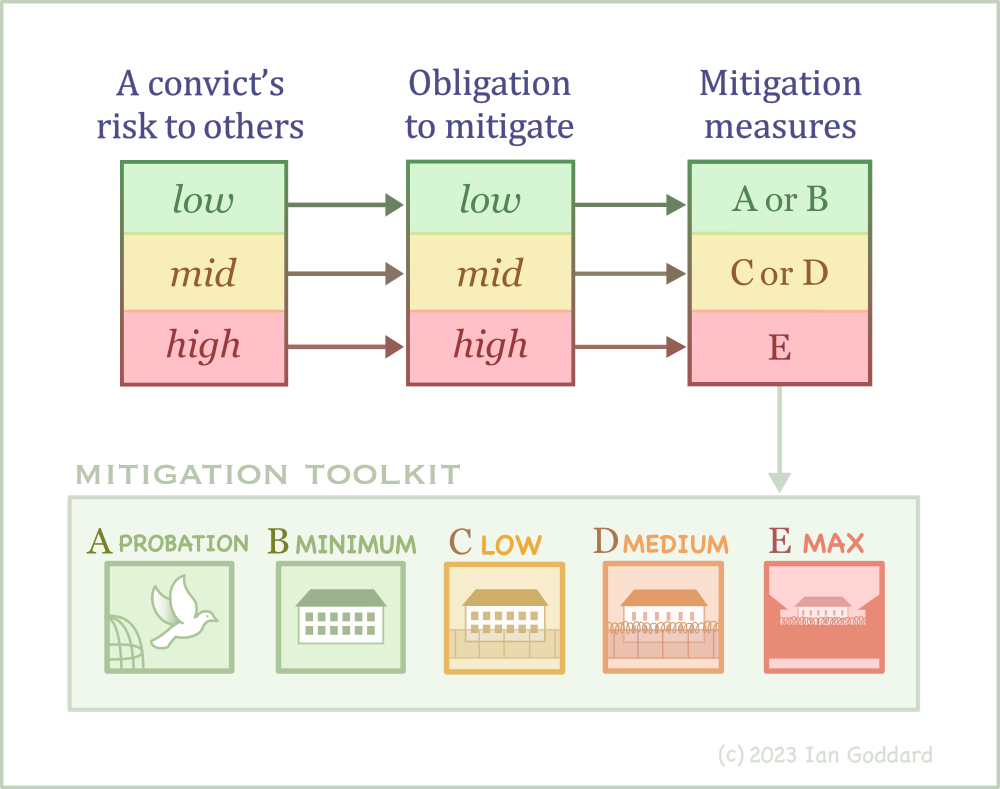
This proportionality framework is robust across domains of risk. For example, public officials have an ethical duty to protect the citizenry from harm posed by criminal convicts whose risk to others varies from lower or higher. That gradient of risk entails a proportional gradient of duty to mitigate that risk with a proportional gradient of measures from probation to incarceration in lower to higher security facilities. This proportionality is illustrated in Figure 4.
Let us consider a third instantiation of the proportionality framework, this time into the risk domain of firearm ownership. If you own a firearm, you incur an ethical duty to mitigate the risk of harm it poses to others, which includes a duty to store it safely. Your stored firearm poses a high risk of harm to others if children or someone with harmful intent finds it. A stored firearm owned by someone who lives alone probably poses less risk to others than one owned by someone who lives with others especially kids. This gradient of risk and duty entails a corresponding gradient of mitigative measures as illustrated in Figure 5, which instantiates the proportionality framework into the domain of firearms-risk management.
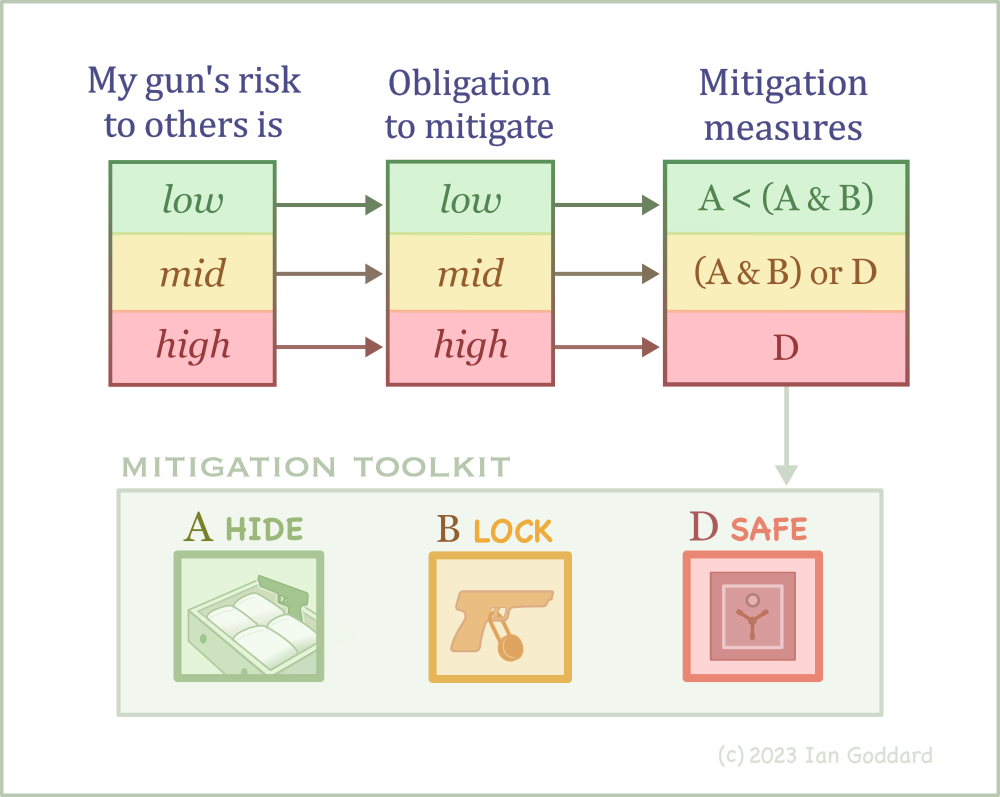
These examples in Figures 4 and 5 show that the respiratory ethics framework in Figure 3 is an instance of the meta-framework of risk mitigation depicted in Figure 2. It is intuitively logical that if we should not cause physical harm to others, then our ethical obligation to take actions required to prevent causing physical harm to others should scale proportionally with the magnitude of the risk of such harm we pose to others. If we pose little risk of physical harm to others, our obligation to mitigate that risk is low and so at most we need only take simple and easy measures to mitigate that low risk. However, as our risk of causing physical harm to others increases, it is both intuitive and logical that our obligation to mitigate that risk increases proportionally, which in turn entails we ought to apply proportionally more vigorous measures to mitigate that greater risk.
Other variables affecting respiratory ethics
The framework for respiratory ethics in Figure 3 accommodates the basic variables regarding the likelihood that you are infectious. However, in various contexts other variables can influence decision making about respiratory ethics, including, (1) the vulnerability of others around you to severe infection outcomes, (2) the prevalence of masking among others around you, and (3) the presence of masking policies. These additional three variables are considered in Figure 6, forming three decision matrices. Let us consider each contextual case.
In the first case, suppose you are planning to visit a nursing home whose residents have a higher risk of suffering significant harm from infections. In that case the risk you pose to these specific other people around you has increased compared to the risk you pose to the average person you encounter outside the nursing home in the unlikely, albeit not impossible, chance that you are asymptomatic and infectious. Now you have a reason to decide that you should wear a mask to protect nursing-home residents even if you believe you are probably not infectious.
In the second case, if most people around you are masking, it may be reasonable to infer that most of them prefer to not breathe your respiratory effluent. You may, therefore, decide to recognize and respect that implicit common consent and don a mask even if you believe it is unlikely that you are infectious.
In the third case, if there is an institutional masking advisory or mandate — for example, if a nursing home requires visitors to mask — you may choose to wear a mask even if you feel fine. And you may choose to do so not merely because you wish to follow rules, but because the existence of such policies probably corresponds to actual higher levels of risk you pose to others under the particular circumstances that brought about out such policies.
Is ethical obligation variable?
It might seem that the magnitude of ethical obligation is actually the same irrespective of the magnitude of risk. For example, you should mitigate low risk with easy measures and you should mitigate higher risk with stronger measures and that can seem like the same magnitude of obligation applies to different levels of risk and the only stratification of levels at hand are the levels of measures you should take, but not levels of ‘shouldness’. If there are no levels of shouldness, the proportional framework in Figures 2-5 is inaccurate. However, it is easy to disabuse oneself of that impression by considering the different moral blameworthiness for failing to mitigate high risk versus low risk. If it is more unethical to fail to mitigate high risk, then ethical obligation itself does in fact range from less to more.
Consider for example person A and person B who both know they should store their handgun in a secure location. And suppose A lives alone and is the only person in her house and she leaves her handgun unattended out on a table in her house, while B is a father living with his young children who have friends over and he leaves his handgun unattended out on a table in his house. Are both due the same magnitude of moral censure for failure to mitigate risk? Of course not! Person B is obviously due far harsher moral reprimand for his failure to mitigate the risk his firearm poses to others. Yes, both should mitigate risk (what seems the same), but person B is uniquely under a higher magnitude of shouldness. Person B must mitigate the risk they pose to others whereas A merely ought to.
Let us consider another example. Suppose person A and person B both know you should cover coughs and sneezes. And suppose that A feels fine and by all impressions is probably not infectious, while B is obviously sick and he believes he’s probably infectious. Now suppose both fail to cover a sneeze in close proximity to others. Are both worthy of equal moral censure? No! Obviously person B is most worthy of reprimand because there is good reason to believe the risk they pose to others is higher. That differential magnitude of moral reprimand is precisely a differential magnitude of shouldness, confirming a gradient nature of ethical obligation.
So, upon reflection it is easy to see that the ethical duty to migrate risk does in fact vary from being less to more obligatory corresponding proportionally to lower and higher risk. So the variation in degrees of ethical obligation in the middle set of the proportionality framework in Figures 2-5 is an accurate model of how ethical obligation exists in real life.
Summary
Motivated by ethical questions arising from the Covid-19 pandemic, the respiratory ethics framework presented here addresses questions about why, how and when we should modify our practices of respiratory hygiene, as for example by donning a face mask. This framework is grounded in the moral principles of nonmaleficence, or non-harm, beneficence and respect for personal autonomy. From the nonmaleficence principle we derive a duty to engage in beneficent action for the benefit of others by acting to protect them from our own respiratory infections. Because this framework relies on a person’s own assessment and mitigation of their risk to others rather than on top-down enforcement, it respects personal autonomy.
From a proportionality framework depicted in Figure 2, wherein increasing risk of harm to others entails increasing ethical obligations to mitigate that risk with increasingly efficacious measures, the framework’s basic decision model is instantiated in Figure 3. The framework is then extended into two-dimensional decision matrices in Figure 6 to guide ethical decision making in more complex contexts. Figures 4 and 5 show how the generalized proportionality framework in Figure 2 can be instantiated in other domains of risk for decision making therein.
After contemplating the ethics of the airborne transmission of risk during the pandemic, I had a paper presenting my conclusions published in the Journal of Health Ethics. Given the professional-ethics focus of the medical-ethics journals, my paper is unique in presenting a personal-ethics framework applicable to everyone. From my survey of the literature, this might be the only formal ethical framework for airborne infectious respiratory disease.
Citation for this essay: Goddard, I. W. (2023). Frameworks for respiratory ethics. Goddard's Journal, December. @ https://iangoddard.com/respiratory-ethics.htm
my inquiries
my home page